Ontario’s home care crisis isn’t coming—it’s already here. While conversations often focus on hospital overcrowding or long-term care waitlists, a quieter emergency is unfolding in living rooms, kitchens, and spare bedrooms across the province.
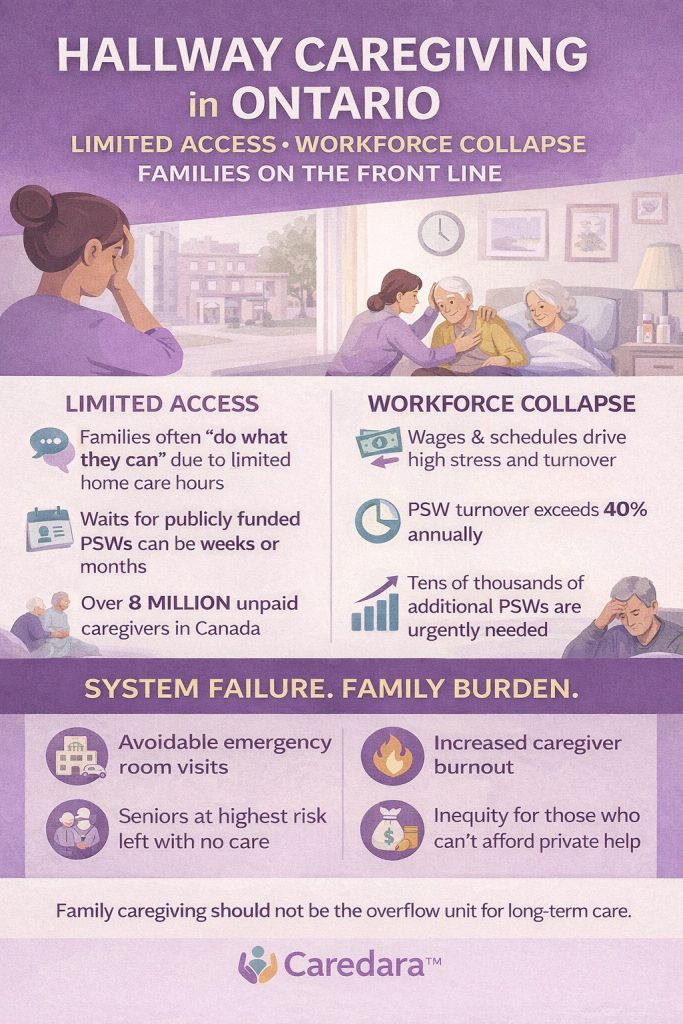
It’s called hallway caregiving—and in Ontario, it’s being driven by two forces colliding at once:
minimal access to care and a rapidly depleting workforce.
A System with Fewer Doors Open
For many Ontario families, accessing home care today feels less like a service and more like a lottery.
Consider the reality:
- Over 8 million Canadians are unpaid caregivers, with Ontario representing a significant share
- Publicly funded home care hours are often limited, delayed, or capped, even for high-needs seniors
- Families routinely report waiting weeks or months for consistent PSW support
- Eligibility does not guarantee availability
As a result, families are told—implicitly or explicitly—to “do what you can” until help arrives.
That waiting period is hallway caregiving.
Workforce Depletion: The Invisible Accelerator
Ontario’s caregiving crisis cannot be separated from its workforce crisis.
- PSW turnover rates exceed 40% annually
- Thousands of trained caregivers are leaving the sector due to:
- Burnout
- Inflexible schedules
- Low wages
- Lack of autonomy and recognition
The province will need tens of thousands of additional PSWs over the next decade just to meet baseline demand
When caregivers leave, access collapses—and families step in to absorb the shock.
Hallway caregiving isn’t just about demand.
It’s about supply disappearing.
What Hallway Caregiving Looks Like Today
In Ontario homes, hallway caregiving shows up as:
- Adult children managing dementia behaviors between work calls
- Spouses providing overnight supervision without relief
- Families coordinating care hour by hour, hoping no one gets sick or injured
- Seniors discharged from hospital with complex needs and minimal follow-up
Care is happening—but not in a system designed to support it. Instead, it’s happening in the margins.
The Cost of Minimal Access
When access to care is scarce, consequences ripple outward:
- Emergency departments fill up with preventable visits
- Hospital readmissions increase
- Caregiver burnout accelerates
- Workforce participation drops as family members reduce hours or leave jobs
- Equity gaps widen, as only some families can afford private support
Hallway caregiving becomes normalized—not because it works, but because it’s the only option left.
Why This Is a System Failure, Not a Family One
Families are not failing the system.
The system is failing to meet reality.
Ontario’s population is aging faster than its care infrastructure can respond. Models built around rigid schedules, limited hours, and centralized control no longer align with how care is actually needed—or delivered.
Hallway caregiving is the symptom of that mismatch.
A Different Way Forward
Addressing hallway caregiving in Ontario requires rethinking how care is accessed and delivered:
- Flexible, on-demand care models that reflect real-world needs
- Support for caregivers, not assumptions of unlimited capacity
- New workforce models that restore autonomy and sustainability for practitioners
- Technology-enabled access that reduces wait times and friction
- Integration across hospital, home, and community care
Care must meet people where they are—not where the system wishes they were.
Naming the Crisis Changes the Conversation
Hallway caregiving gives language to what families already feel:
being stuck between responsibility and exhaustion, between love and limits.
And in Ontario—where access is shrinking and the workforce is thinning—that language matters more than ever.
Because until we acknowledge hallway caregiving as a system outcome, not a personal failure, the crisis will remain invisible.
And invisibility is the most dangerous place for care to live.